See this article by Emry president Derek Fitteron as it originally appeared on Industry Today.
Manufacturers understand the importance of providing their employees with reliable and cost-effective health coverage. It’s one of the ways manufacturing maintains a lower turnover rate than most other industries.
But as healthcare costs rise, providing excellent benefits is getting harder for manufacturers to do. High-deductible health plans (HDHP) serve as a solution for manufacturers who employ large numbers of part-time, seasonal or lower-wage workers. One example of a HDHP is a Minimum Essential Coverage (MEC) plan, which is a type of health insurance plan that meets the requirements of the Affordable Care Act (ACA).
MECs provide an affordable way to extend some level of healthcare coverage in lieu of increasingly expensive comprehensive plans. But MEC plans often make individuals susceptible to incurring medical debt because of the high deductibles and out-of-pocket expenses. A crucial tool in the fight against medical debt for those with HDHPs is the healthcare benefit navigator, which protects employees from exorbitant costs while also ensuring they fully comprehend and optimally utilize their coverage.
Streamlining health coverage communication
Healthcare plans, including MEC plans, involve a degree of complexity that can leave employees feeling overwhelmed and underinformed. MEC plans often offer more limited coverage, leaving employees with numerous questions about what is included and what isn’t. It’s often these types of misunderstandings that lead to increased costs and debt. Lack of clarity also causes individuals not to seek preventative and problem-focused care early, leading to higher costs later.
A healthcare navigator acts as a bridge between employees and their healthcare benefits. By being on hand to answer questions, explain coverage and demystify healthcare jargon, navigators alleviate the pressure on the human resources team, allowing them to focus on other critical aspects of the business. And most importantly, employees feel supported and understood in their healthcare journey. Having this support also means employees don’t have to spend time during the day making calls to insurers or healthcare providers, or spend time tracking down prescriptions, which improves productivity.
For example, MEC plans typically have a high deductible before certain types of care are covered. Even seeking care from in-network providers can leave employees with large out-of-pocket costs. A procedure such as an MRI might cost $400 at one location and $1,600 at another. If the deductible hasn’t yet been met, the employee could be paying the full amount. Benefit navigators make it easier to comparison shop in a way that most healthcare consumers simply don’t realize is necessary until an unexpectedly large bill arrives.
Boosting employee satisfaction and retention
Competitive benefits packages play an essential role in retaining employees, especially in the manufacturing industry where workers have a multitude of options. Unfortunately, unexpected and high healthcare costs can leave employees feeling unsupported and potentially seeking alternative employment.
Pre-care support helps employees understand and plan for the cost of their healthcare, guiding them toward affordable care options covered by their MEC plan before any liability is incurred. By ensuring that employees feel secure in their healthcare choices, a company enhances its reputation as a caring and supportive employer, ultimately increasing retention rates and boosting its standing in the manufacturing industry as a whole. These navigation services also help increase satisfaction with the benefit plan.
Bringing awareness of ways to save
Hospital financial assistance programs — which every nonprofit hospital in the United States is required to offer — are a great example of how benefit navigation supports employees’ financial well-being as they navigate the healthcare landscape.
These programs provide free or discounted care to income-eligible patients. But awareness of hospital financial assistance programs is lacking — even when one hospital visit can be enough to wipe out a family’s savings and push them into bankruptcy.
The exact numbers and percentages change depending on the individual hospital and which state a patient is in, but even households with income up to 400 percent of the federal poverty line may be eligible to receive financial assistance. In hard numbers, this means a family of four with an annual income of $120,000 may qualify. A high percentage of manufacturing employees are eligible for these programs, but many don’t realize it.
Some emergencies can’t be avoided, but when there’s enough time for an informed choice to be made, choosing the right hospital may mean the difference between receiving free care or falling into financial ruin. Plus, patients can apply for financial assistance even after receiving care. Healthcare benefit navigators can assist in the process, encouraging those eligible to apply.
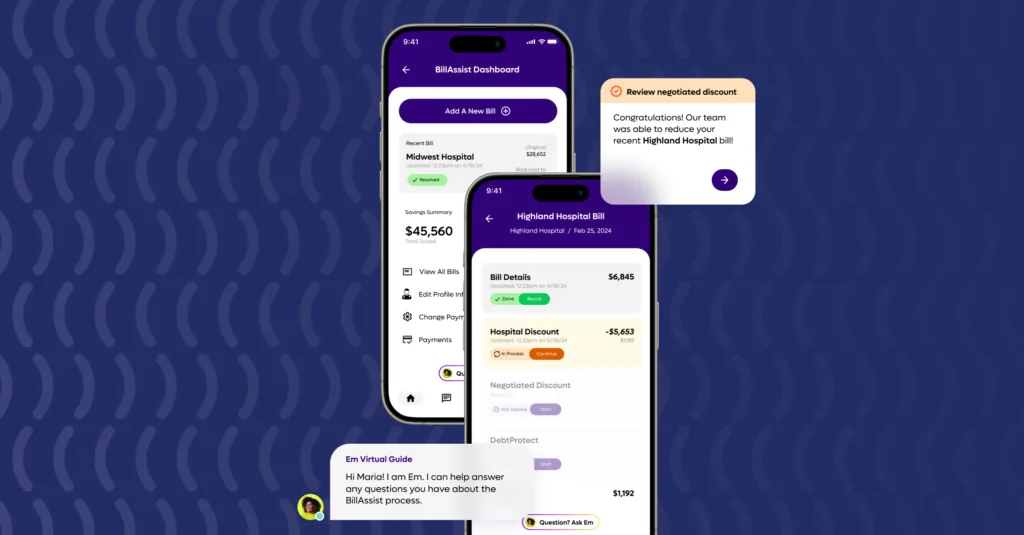
Employees who don’t qualify for financial assistance still want to save money. A good navigator can negotiate a reduction in the out-of-pocket costs that accompany high deductible healthcare or negotiate a payment plan to extend payment over time.
Empowering employees with advocacy
Unexpected and expensive medical bills and complicated healthcare paperwork can be daunting. A healthcare navigator acts as an advocate for employees, helping guide them through these challenges.
From negotiating lower out-of-pocket costs to identifying potential billing errors, this type of support can result in significant savings for employees. Not only does this foster trust between employees and the company, but it also contributes to a more positive perception of their overall benefits package.
While MEC plans offer an affordable health insurance solution for manufacturers, they can also present challenges for employees trying to navigate the healthcare system. Incorporating a healthcare navigator into a benefits strategy not only optimizes the value of MEC plans for employees, but also reinforces the company’s commitment to employee well-being.